 Recent studies have found statistical links between pesticide use and an outbreak of Parkinson's disease in California farm towns. Researchers even know which chemicals are the likely culprits. What's the government doing about it? Not much.
Recent studies have found statistical links between pesticide use and an outbreak of Parkinson's disease in California farm towns. Researchers even know which chemicals are the likely culprits. What's the government doing about it? Not much.
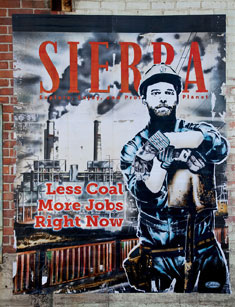
published in Sierra Magazine
Bruce McDermott tosses me the keys to his pickup, and I hoist his chrome walker into the truck's bed. "You need to see this," he tells me as he angles his torso and braced leg into the cab, then slams the door.
It's a rainy fall day in the Central Valley town of Visalia, California, and McDermott wants to show me some of the houses of people here who've been diagnosed with Parkinson's disease, the incurable neurodegenerative affliction that, coupled with a recent car crash, has left him unable to drive. I've never been at the wheel of such a behemoth truck before—or one with shotgun shells in the door well, for that matter—but I know better than to argue. McDermott was once the city's chief of police; when he makes suggestions, people tend to say, "Yes, sir."
A big, friendly bear of a man who likes to joke that his doctor calls him "fat boy," McDermott wears khaki shorts, sandals, and a crisply pressed polo shirt. Diagnosed with early-onset Parkinson's, he was forced to retire from the police force in 1997, at age 46, after he tried to place his right hand on the Bible to swear in a new officer but his arm shook so uncontrollably that people thought he was waving hello.

As we near his boyhood home on Border Links Drive, McDermott points to the house next door, where his godfather, a prominent attorney, died three years ago from complications of Parkinson's. Nearby, he shows me a field where crop dusters once landed their planes and routinely dumped their tanks. In a half-mile stretch, McDermott points to four homes where residents have been diagnosed with the disease.
Some neurologists dub the 300-mile-long string of Central Valley farm towns between Bakersfield and Sacramento "Parkinson's Alley," and recently released statistics back them up. A study published last year by researchers at the University of California, Los Angeles, found that Central Valley residents under age 60 who lived near fields where the pesticides paraquat and maneb had been used between 1974 and 1999 had a Parkinson's rate nearly five times higher than other residents in the region.
I steer McDermott's truck into the driveway of his friend Margaret Haworth, a former tennis player and expert skier. Like McDermott, Haworth suffers from early-onset Parkinson's; she was diagnosed 16 years ago, at age 49.
Our visit is a surprise, but Haworth welcomes McDermott as if he's family. As he slowly makes his way up her front steps, she says of his walker, "I see you got a new hot rod."
Haworth tells us her mother was also afflicted by Parkinson's but never spoke of it. McDermott nods; it's a familiar story. "A lot of people in the valley won't tell you they have Parkinson's disease if they do," he says. "I know doctors who would lose their license if their insurance carriers knew they had it."
Research into the link between pesticides and Parkinson's in the Central Valley dates back to 2000, when UCLA epidemiologist Beate Ritz began comparing mortality records with pesticide-application reports. She discovered that California counties reporting the highest pesticide use also had the highest rates for Parkinson's-related deaths. Examining agricultural records from 1989 to 1994, Ritz found that when insecticides were applied to more than a third of a county's acreage, the risk of its residents' dying from Parkinson's disease increased 2.5-fold. She also found studies that revealed that as many as 40 percent of the area's Parkinson's cases are never mentioned on death certificates, possibly because many migrant workers fail to report the disease, or move on before symptoms arise.
The police chief retired after a swearing-in ceremony in which his hand shook so badly that people thought he was waving hello.
Ritz and her research team found that Central Valley residents who consumed private well water and lived within 500 feet of farmland with documented long-term pesticide use were almost twice as likely to get Parkinson's disease. Their 2009 report, produced under the auspices of the federally funded Parkinson's Environment and Genes Study, was the first to quantify residents' exposure to such chemicals by comparing land-use maps with state-mandated pesticide-application records. "We're seeing effects not just on people in their homes but also on farms and in workplaces," Ritz told me in Los Angeles before I traveled 200 miles north to meet with McDermott.
Visalia, a 160-year-old gold rush town, has grown by more than a third to about 120,000 people in the past decade. It's in the heart of the Central Valley—the vast farm belt west of the Sierra Nevada where about 7 percent of the nation's crops are grown, producing $20 billion in annual revenues. Growers here use about 115 million pounds of pesticides every year.
Some of those pesticides are finding their way into residential water supplies in accumulations that surpass government safety standards, according to a number of studies—including tests of private-well samples gathered exclusively for this article. More than 1 million people in the region have tap water that isn't safe to drink because of nitrate contamination from manure, fertilizers, and leaking septic tanks, according to a collaborative report by the Pacific Institute, Visalia's Community Water Center, the Clean Water Fund, and California Rural Legal Assistance Foundation. Most of those residents are from low-income and Spanish-speaking households.
More than half of Central Valley communities rely on water stored underground for their drinking supply, the Community Water Center reports. Recent groundwater sampling found that the water in 75 percent of the private domestic wells in Tulare County, of which Visalia is the seat, contains unsafe levels of nitrates.
"We pay twice for water each month," says Susana DeAnda, the center's co-executive director. "Once for contaminated well water and once for bottled water."
Nitrates can also be a sign of pesticide contamination, but testing for pesticides in drinking water is expensive and not mandated. Some testing is done, however, and last year the State Water Resources Control Board released the results of a domestic-well-water survey in Tulare County; pesticides turned up in 13 of 19 wells sampled.
 By the time I park McDermott's truck in his driveway, the rain has stopped. Gripping his walker, he shuffles back inside his home. The walk leaves him breathless. A lifelong Republican who favors Fox News, McDermott says he had long assumed that, in America, if something was wrong, it would be fixed. Now he's not so sure.
By the time I park McDermott's truck in his driveway, the rain has stopped. Gripping his walker, he shuffles back inside his home. The walk leaves him breathless. A lifelong Republican who favors Fox News, McDermott says he had long assumed that, in America, if something was wrong, it would be fixed. Now he's not so sure.
"It's an ugly thing when you look at it and think maybe something could be done to prevent this," he says. "I'm convinced it's exposure to the environment. Something's going on here."
Currently, no federal or state water quality standards regulate domestic well water in California, even though private wells are the primary source of drinking water for 1.6 million people in the state and more than 43 million, or 15 percent of the population, nationwide. The federal Safe Drinking Water Act covers public water supplies, but Congress never extended the law to include private wells, which can be more susceptible to contamination because they tend to draw from shallower aquifers and often are close to farms that use pesticides.
The federal Clean Water Act largely exempts normal agricultural activities from regulation. California's Safe Drinking Water Act monitors water coming out of the tap but doesn't regulate the source. Although statutes are in place mandating the state to monitor and regulate agricultural pollution in drinking water, the program has yet to be implemented, according to Community Water Center cofounder Laurel Firestone. In California, the state Department of Pesticide Regulation conducts an annual survey of some domestic wells. Last year, for example, state regulators tested 136 wells and found pesticides in 103 of them. But the agency keeps the location of its testing confidential, citing concerns about terrorism.
"Nobody is testing domestic wells in any systematic way," says Robert J. Gilliom, a hydrologist and the head of pesticide studies for the U.S. Geological Survey's water quality assessment program.
Since Ritz's UCLA research was based on historical data, I wanted to know what pesticides are in the water now. But no one could tell me. So, I ordered some water-testing kits and set out to answer two simple questions: What pesticides are present in Central Valley well water and are any of them implicated for Parkinson's disease? The lab results revealed a potentially harmful mix of herbicides in tap water from 6 of the 10 private wells I tested. (See "Testing for Pesticides".)
"We pay twice for water each month. Once for contaminated well water and once for bottled water."
Of course, not everyone wants to know what's in his or her water. When I arrived at a walnut farm in Visalia to take water samples, I asked the grower—whose hand shook from Parkinson's—what pesticides he used on his property. He said, "Whatever the gestapo lets us use."
"I'm dying to know, but I also am afraid to find out," the widow of a Parkinson's victim told me when I asked if I could test her drinking water. Her husband had worked for a program that advises farmers on how to use pesticides, and the couple had lived on a citrus ranch for more than 40 years. He sometimes came home "up to his elbows in the stuff." She told me I could take water samples on the ranch, but only if I didn't reveal her identity.
 Off a country road outside Hanford, about 20 miles west of Visalia, I dropped by the home of Peggy and Jim Greaser to take a water sample from their kitchen sink. Their living room window has a view of the cornfield next door. Both Peggy and Jim, a former Sears technician, complained that the "drift" from crop dusters often burns their eyes and has ruined the paint job on their car.
Off a country road outside Hanford, about 20 miles west of Visalia, I dropped by the home of Peggy and Jim Greaser to take a water sample from their kitchen sink. Their living room window has a view of the cornfield next door. Both Peggy and Jim, a former Sears technician, complained that the "drift" from crop dusters often burns their eyes and has ruined the paint job on their car.
Jim, now a part-time DJ known as Jim Dee on K6RGZ, suffers from Parkinson's disease. He drives a motorized cart from his front door to a nearby shack that houses his radio studio. Leather straps hang from shelves crammed with tape decks and vinyl records, so he has something to grasp.
"You start losing your walking ability," he said. "I've fallen so many times I've lost track."
Parkinson's, one of the most intractable of all neurological diseases, afflicts 500,000 to 1.5 million people in the United States. It's caused when nerve cells die in the area of the brain that produces dopamine, a neurotransmitter that's essential to everything from moving muscles to feeling pleasure. As dopamine levels decrease, messages that control motor function are blocked.
Although symptoms have been mentioned in texts dating back to biblical times, the disease was officially "discovered" in 1817, when British physician James Parkinson first described the "shaking palsy." But it wasn't until the mid-1980s that scientists stumbled on a link between pesticide exposure and Parkinson's disease, thanks to a bizarre outbreak among heroin addicts and an astute young San Francisco Bay Area neurologist named J. William Langston.
Langston, now scientific director at the Parkinson's Institute in Sunnyvale, California, had been asked to examine a cluster of young patients who looked like living statues; they could neither move nor speak and appeared to be in the advanced stages of Parkinson's disease. He learned that all of them had injected a new form of synthetic heroin. Alarmed, he called a press conference to alert the public to his "frozen addicts" and warn of bad drugs on the streets. When he prescribed levodopa, which is used to treat Parkinson's, the addicts, whose faces were so stiffened that they drooled uncontrollably, soon found that their symptoms abated.
The illicit drug they'd taken contained a compound known as MPTP, which has a similar chemical structure to that of paraquat—one of the most widely used herbicides in the world. Paraquat is of particular concern to Parkinson's researchers because of its synergistic effect, particularly when used with the fungicide maneb.
Taking their cues from Langston's earlier work, Ritz and her team discovered that long-term exposures to paraquat and maneb caused an eightfold increase in the development of Parkinson's for people under age 60. Paraquat was banned by the European Union in 2007 but is still widely used in the United States; about 75,000 pounds of it are applied annually to alfalfa, grapes, and other crops in Tulare County. The EPA banned maneb for use on corn, grapes, and apples in 2005 but continues to allow its use on almonds, which are abundant in the Central Valley.
Another chemical of particular concern to Parkinson's researchers is the fungicide ziram. When the EPA proposed prohibiting ziram use on 35 crops in 2003, a plant pathologist with the U.S. Department of Agriculture insisted that the pesticide had a "clean bill of health" and said workers could protect themselves by wearing "long pants and long sleeves." But cell studies by the UCLA researchers and others have shown that ziram kills certain brain cells whose absence leads to Parkinson's, and the UCLA team found that people exposed to the fungicide for 25 years or longer have a three-times-greater chance of developing the disease.
In 2008, California regulators placed ziram on their risk-assessment "priority" list. Four years later, no one's followed up.
"We have no estimated date for the assessment," Lea Brooks, communications director with California's Department of Pesticide Regulation, told me. "Our work schedule is behind due to furloughs, retirements, and a hiring freeze. It's on the priority list for a risk assessment, but there is no timeline."
Once a Month for the past 10 years, neurologist Jeff Bronstein has left his hillside home in Los Angeles at four a.m. to drive more than 150 miles north to the Central Valley, where he meets with Parkinson's patients before they take their daily medications, which mask symptoms. As part of the UCLA Parkinson's research team, Bronstein, a professor of neurology and molecular toxicology at the university's David Geffen School of Medicine and director of its Movement Disorders Program, needs to make sure that patients enrolled in the Parkinson's Environment and Genes Study have been correctly diagnosed (since it's easy to mistake other neurological symptoms for those of Parkinson's disease) and to chart their progress.
Over the years, Bronstein has met with farmworkers, corporate executives, police officers, college professors, and, of course, pesticide applicators. Although he lacks irrefutable evidence, he is convinced that pesticides are the culprit behind his patients' affliction.
"It's worth it," he told me of his five- to seven-hour round-trip commutes. During one of them, he spoke to me on his car phone as a crop duster roared overhead. "How many years did it take to prove smoking causes lung cancer? That's where we are with pesticides. The onus is on us to prove this stuff is bad. And what's really goofy is that what's considered an 'acceptable' level is completely arbitrary. They come up with numbers based on acute toxicity. But it's years and years of low-level exposure that matter, not acute toxicity. You need to look at chronic exposure before any meaningful discussion can take place."
DeVries has begun to display symptoms that suggest she has Parkinson's. "My doctor told me not to worry, but how can I not?"
In 2007 the U.S. Department of Agriculture partnered with the EPA to begin testing for pesticides at extremely low concentration levels in domestic well water. In 2009, the agencies took samples from 278 domestic, school, and farm wells in 16 states and detected pesticides in 152, or 45 percent, of them. "In the future, we'll see more and more pesticides in groundwater," said hydrologist Terry Councell, who runs the USDA's water monitoring program. "A lot of these pesticides haven't even hit the water table yet."

One morning I meet over coffee with Donna DeVries, former president of the Central Valley Parkinson's Disease Support Group. DeVries, a 57-year-old dental office manager, tells me she spends the first Friday of every month at the local Methodist church, with the Visalia-based support group, which ranks second in the United States in fundraising. She spent years caring for her father and father-in-law, both of whom died after battling the disease.
"All of our doctors have told us, 'Move. Get out of the valley. It's not a healthy place to be,'" she says. As she speaks, she sits on her right hand to control its shaking. She suspects she has Parkinson's too. "My doctor told me not to worry about it, but how can I not?"
 Several dozen people attend the support group's Friday-morning meeting, and the conversation ranges from sharing medication tips to dealing with the inevitable depression that accompanies the disease. "I told my wife, 'Put the guns in the safe,'" says a man in his 40s who has driven several hours to be here.
Several dozen people attend the support group's Friday-morning meeting, and the conversation ranges from sharing medication tips to dealing with the inevitable depression that accompanies the disease. "I told my wife, 'Put the guns in the safe,'" says a man in his 40s who has driven several hours to be here.
Not everyone is keen on such frank talk, though. Bruce McDermott, for one, swore off the group after he sat through a downer of a discussion about morticians. He likes to think of Visalia as a "roll-up-your-sleeves kind of town" where people who share his disease can live a normal life, and where he and others can change the future for the better by verifying—and publicizing—a link between pesticides and Parkinson's.
"If I can help one person," McDermott says, "I feel good."
 |
 |
 |
published in Sierra Magazine



